Did you know your body contains nearly 100 trillion bacteria—outnumbering your own human cells ten to one? These invisible allies, known collectively as your microbiome , are quietly working around the clock, influencing everything from digestion and mood to your long-term health. This comprehensive guide unpacks the hidden ecosystem inside you , revealing jaw-dropping facts, proven strategies, and simple steps you can use today to transform your gut health. Whether you’re curious about probiotics, searching for real-world success stories, or want to unlock the secrets to lifelong wellness—the magic starts in your gut.
Shocking Facts: How the Microbiome Shapes Your Wellbeing
- Nearly 100 trillion bacteria , known as the microbiome, inhabit the human gut—outnumbering human cells by ten to one. These microscopic organisms control far more than digestion.
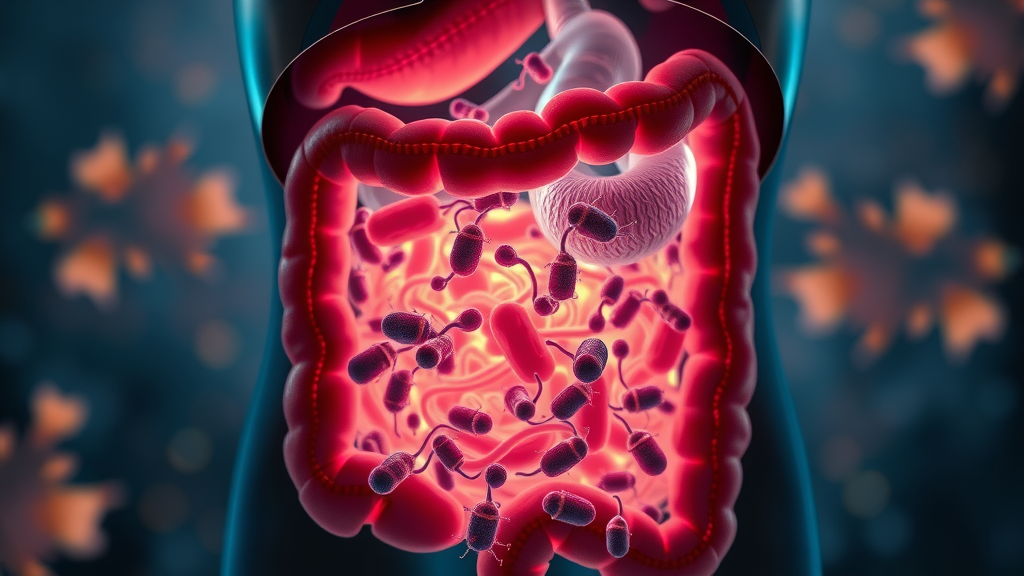
The microbiome is a complex network of microorganisms—including bacteria, viruses, and fungi—that form the backbone of your gut health . What’s truly startling is that these trillions of microbial inhabitants don’t just reside in your digestive tract; they actively communicate with your immune system , influence your mental wellness, and even determine how you absorb vital nutrients and synthesize fatty acids and amino acids . Many leading health experts, including those at the Cleveland Clinic , agree that the health of this microbial community is integral to nearly every aspect of the human body .
Scientific studies have shown that disruptions to the gut microbiome can lead to wide-ranging consequences—everything from chronic inflammation, weight gain, and irritable bowel syndrome (IBS) to weakened immunity and mood disorders. In essence, the human gut operates like a biological command center, and its microbial makeup often predicts your susceptibility to illness and your resilience against disease. Understanding and nurturing these hidden allies may be the most powerful step you ever take toward optimizing your health and vitality.
Why Nurturing Your Microbiome Matters More Than Ever

- The latest research on microbiomes and chronic disease
- Practical examples of changes in gut health
- Impact on energy, immunity, and mood
- Microbiome’s role in prevention and longevity
The importance of a balanced microbiome has skyrocketed in recent years as scientists uncover its role in conditions ranging from metabolic syndrome to autoimmune diseases . Chronic stress, processed foods, and overuse of antibiotics are all factors in our environment that can threaten this delicate internal ecosystem. Experts at the Cleveland Clinic have found that supporting healthy gut bacteria not only bolsters physical defenses but also can profoundly affect mood stability, daily energy, and overall vibrancy.
Small changes—such as incorporating more fiber-rich foods and fermented products into your diet—can trigger marked improvements in gut health within weeks. Imagine waking up with increased energy, clearer skin, and fewer digestive disturbances. People who focus on supporting their gut microbiome often report enhanced mental clarity, improved resistance to illness, and a stronger sense of wellbeing. In a world where chronic illness is increasingly common, proactive microbiome care is your best insurance policy for long-term health.
What You'll Gain From Mastering Microbiome Science
- Actionable microbiome optimization tips
- Science-backed gut health strategies
- Deeper understanding of your gut microbiome’s role in health and disease
When you invest in learning about the microbiome , you’re doing much more than reading a health trend. You’re arming yourself with science-backed strategies that can help prevent obesity, boost your immune system , and lower your risk of digestive and autoimmune conditions. With practical tips such as incorporating specific probiotics and prebiotics, monitoring your symptoms, and staying attuned to current research, you’ll gain daily control over your health destiny.
A key outcome is being able to recognize early signs of imbalance (like digestive trouble or mood swings) and knowing exactly how to address them—empowering you to respond before small issues become chronic problems. This deeper level of awareness separates those merely chasing wellness fads from true masters of their gut health . You’ll also understand how good habits reinforce a dynamic, resilient gut microbiome , setting you up for a healthier, happier future.
Defining the Microbiome: The Complex Ecosystem Within
What is the microbiome and how does it function?
- Relationship between gut microbiome, gut microbiota, and human gut
- Anatomy of gut bacteria and the broader microbiome
- Cleveland Clinic insight on gut health
The microbiome refers to the collective community of bacteria , viruses , fungi , and other microscopic organisms living within and on the human body , with the largest congregation found in the gastrointestinal (GI) tract . Nested within your intestinal tract , the gut microbiome specifically describes the trillions of microorganisms living inside your digestive system. They form a highly organized and mutually beneficial ecosystem sometimes referred to as the “forgotten organ” because of its profound impact on health.
Functionally, the gut microbiota are directly involved in breaking down dietary fibers, producing essential fatty acids and amino acids , synthesizing vitamins, and regulating immune system activity. According to the Cleveland Clinic , a healthy microbiome doesn’t just ensure comfort after meals. It helps prevent inflammation, supports metabolism, and plays an important role in resisting infection and disease. The dynamic interplay between microbial communities and the cells of the human gut shapes everything from your digestive efficiency to your mental outlook.
"The microbiome is the foundation of human health—when you nurture it, your whole body flourishes."
Unlike static organs, the microbiome constantly adapts in response to your diet, lifestyle, environmental exposures , and even your stress levels. Each person’s microbial ecology is unique, much like a fingerprint. The more diverse and balanced these microbial communities are, the more robust your overall health and disease resistance. It is this dynamic nature that makes the microbiome “magic” to unlock and master.
The Microbiome-Gut Connection: How Your Gut Microbiome Affects the Body
Link between gut microbiome and immune system response
- Gut health, inflammation, metabolism, disease prevention
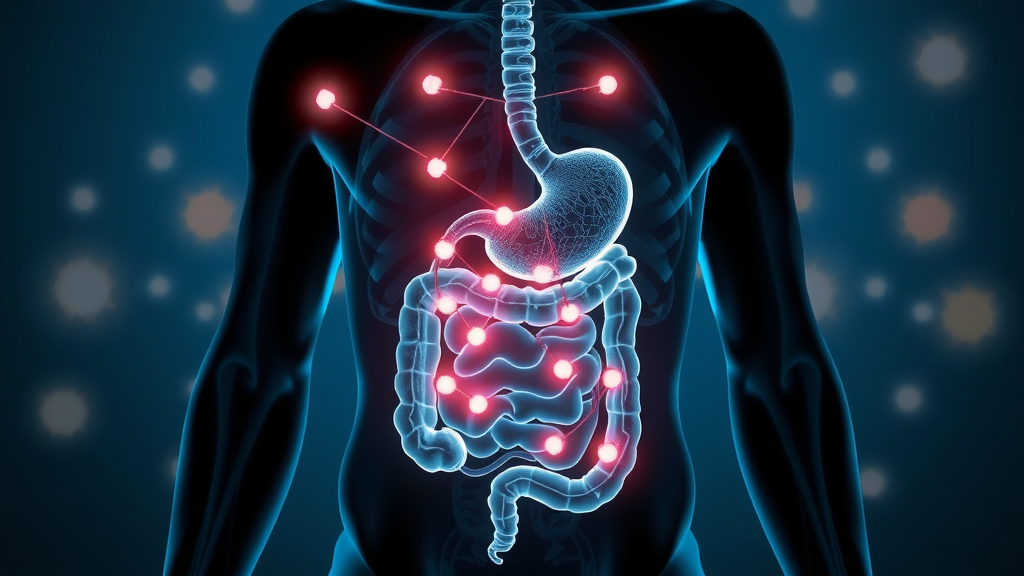
One of the most profound relationships in biology is the two-way connection between your gut microbiome and immune system . Roughly 70% of immune cells reside in the GI tract , strategically placed to interact with the microbiota. Beneficial gut bacteria help train immune cells to distinguish between harmful invaders and friendly antigens, reducing unnecessary inflammation and curbing the development of autoimmune conditions like inflammatory bowel disease .
A healthy gut microbiota helps break down undigested food particles, produces short-chain fatty acids that feed the cells lining your intestines, and acts as a barrier to harmful pathogens. Disruption or depletion of these bacteria, often from antibiotics or chronic stress, can lead to “leaky gut syndrome,” chronic digestive symptoms, and a compromised immune system. In essence, maintaining microbial balance is one of the most important factors in disease prevention and robust gut health .
How gut bacteria influence brain function, mood, and energy
The impact of the microbiome extends far beyond digestion and immunity. The so-called gut-brain axis describes the constant biochemical communication between gut bacteria and the nervous system. Studies have shown that certain probiotic strains can boost the production of mood-regulating neurotransmitters—like serotonin, which is mostly synthesized in the gut. Thus, gut dysbiosis , or imbalance, is strongly linked to mental health disorders including depression, anxiety, and chronic fatigue.
Furthermore, by optimizing your microbiome, you can experience improved focus, sharper cognitive performance, and more reliable energy levels. The microbial community in your gut helps regulate blood sugar, influences nutrient absorption, and modulates hormones that play a key role in your sense of vitality. In short, a balanced microbiome is central to feeling good—both physically and emotionally.
Diversity in the Microbiome: Why More Means Healthier
- Role of gut microbiota
- Examples of diverse gut bacteria
- Why biodiversity sustains human gut
| Type of Gut Bacteria | Key Function | Associated Health Outcome |
|---|---|---|
| Bifidobacterium | Ferment fiber to produce short-chain fatty acids and vitamins | Supports immunity, reduces inflammation, promotes digestive comfort |
| Lactobacillus | Produces lactic acid, supports microbe balance | Prevents pathogenic growth, supports vaginal and gut health |
| Akkermansia | Maintains intestinal barrier integrity | Improved metabolism, reduced risk of obesity and metabolic syndrome |
| Faecalibacterium | Produces anti-inflammatory compounds | Lowers risk of inflammatory bowel syndrome and chronic disease |

Diversity is the hallmark of a resilient microbiome . The more varied your gut microbial population, the more functions are covered—like a well-stocked toolbox for your body. A broad array of species of bacteria ensures the production of essential vitamins, a robust resistance to pathogens, and stronger immune system regulation. Lack of diversity, by contrast, is linked to digestive disorders, weight gain, autoimmune disease, and even skin conditions.
Real-world examples show that traditional diets rich in fruits, vegetables, nuts, and fermented foods foster far greater gut microbial diversity than diets dominated by highly processed foods. By consciously seeking variety—both in what you eat and in your environment—you naturally support the proliferation of the healthiest microbiota. Ultimately, biodiversity in the microbiome sustains the human gut, forming the foundation of optimal gut health .
Signs You Shouldn’t Ignore: Is Your Gut Microbiome Unhealthy?
- Common symptoms: digestive problems, fatigue, skin issues, autoimmune signals, connection to gut microbiome imbalance
Your body often sends subtle—yet clear—signals when your gut microbiome is imbalanced. Digestive problems like bloating, constipation, or frequent diarrhea may point to gut dysbiosis . Skin issues, such as eczema or acne, persistent fatigue, unexplained weight gain, or increased susceptibility to infections and allergies often reflect disruptions deep within the gut bacteria community. According to Cleveland Clinic specialists, many seemingly “random” symptoms are linked to microbial communities in the GI tract.
Ignoring these signs can cause minor imbalances to snowball into chronic issues such as irritable bowel syndrome , inflammatory bowel disease, and even autoimmune conditions. Tune in to your body—and remember, the earlier you identify and address symptoms, the easier it is to restore a healthy gut microbiome and reclaim your energy and wellbeing.
-
5 Warning Signs of an Unhealthy Gut Microbiome (Cleveland Clinic Advice):
- Persistent digestive discomfort (bloating, gas, abdominal pain)
- Unexplained fatigue or poor energy
- Recurring illnesses and infections
- Changes in skin appearance—eczema, rashes, or flares
- New food intolerances or sensitivities
Microbiome Imbalance: What Damages Your Gut Microbiota?
- Effects of antibiotics, stress, processed foods on the microbiome
- Erosion of good gut bacteria, Cleveland Clinic’s warnings
The gut microbiome is exceptionally vulnerable to modern stressors. Repeated or unnecessary use of antibiotics can dramatically deplete beneficial gut bacteria , making space for harmful species. Chronic emotional or physical stress has also been shown to reduce microbial diversity, weakening both your digestive system and immune response. Eating a diet rich in highly processed foods and sugar feeds undesirable bacteria and starves essential microbes, further breaking down the microbial ecology that supports your health.
The Cleveland Clinic points to the danger of environmental toxins—including pollution and chemicals found in household products—as increasingly common factors that erode the integrity of the gut microbiome . Cumulative damage impacts your entire system, from metabolism and weight regulation to thinking, mood, and physical illness. Awareness is the first step; once you identify these risk factors, you can take action to eliminate or limit their effect.
Repairing Your Microbiome: Actionable Steps for Gut Health
How can I repair my microbiome?
- Guidance on prebiotics, probiotics, fermented foods, and dietary changes to restore microbiome

Restoring your microbiome starts with what you put on your plate. Choose fiber-rich vegetables, legumes, and whole grains, which act as prebiotics—fuel for beneficial bacteria. Incorporate probiotic-rich foods such as yogurt, kefir, kimchi, and sauerkraut. These introduce live cultures that help replenish microbial diversity and enhance gut health naturally. Top microbiome researchers and the Cleveland Clinic suggest minimizing processed foods, artificial sweeteners, and unnecessary antibiotics.
Beyond food, embrace lifestyle shifts: get regular exercise, manage stress, and prioritize restorative sleep to foster a healing environment for the gut microbiome . Even small shifts can create dramatic changes in energy, immunity, and mental clarity in just weeks. The magic is in consistency—so start with manageable changes and build from there for optimal gut health .
How do you clean your gut microbiome?
- Detox strategies and scientifically vetted myths vs. facts
Despite marketing claims, harsh cleanses and extreme detox regimens can do more harm than good. Instead, the most effective way to “clean” your microbiome is through gradual, science-backed intervention. Transition toward a diet rich in leafy greens, whole plant foods, and naturally fermented items. Stay hydrated, reduce intake of artificial chemicals, and introduce probiotics gently. Avoid sudden, drastic diet overhauls, which can shock the microbial community and cause digestive distress.
-
Top Foods for Gut Microbiota Restoration (Cleveland Clinic):
- Plain, unsweetened yogurt (live cultures)
- Kefir (fermented milk)
- Kimchi and sauerkraut (fermented vegetables)
- High-fiber foods (lentils, beans, oats, apples, bananas)
- Miso and tempeh (fermented soy products)
Microbiome in Everyday Life: Real-World Success Stories
"After just 4 weeks of focusing on my gut microbiome, my energy and mood improved dramatically—further proof that a balanced microbiome changes lives."
- Case examples: managing IBS, boosting mood, overcoming food sensitivities

The transformative power of the microbiome is more than theoretical. Take, for example, the story of Sarah, who suffered from irritable bowel syndrome (IBS) for years. After introducing more fermented foods, increasing her vegetable intake, and using a daily probiotic as per Cleveland Clinic guidance, her symptoms improved within a month. Her story isn’t unique—many people report significant relief from chronic bloating, abdominal pain, and unpredictable digestion after making targeted changes to support their gut bacteria .
Others find that optimizing the gut microbiome has surprising benefits for mental health and energy. Case studies reveal that individuals struggling with mood swings and chronic stress report lower anxiety and improved concentration after supporting their microbiota. The takeaway? Consistent, microbiome-friendly habits can rebalance health and vitality—no matter where you start.
Science-Backed Microbiome Nutrition: Foods That Feed Gut Health
- Probiotic-rich foods, fiber sources, diversity for optimal microbiome, Cleveland Clinic’s research
| Category | Key Examples | How They Help the Microbiome |
|---|---|---|
| Probiotics | Yogurt, kefir, miso, tempeh, kimchi, sauerkraut | Add healthy bacteria, increase microbial diversity |
| Prebiotics | Bananas, asparagus, leeks, onions, garlic, oats | Feed beneficial bacteria, promote growth and balance |
| Fiber-rich Foods | Legumes, beans, whole grains, berries, apples | Support digestive motility, increase short-chain fatty acids |
| Polyphenol-rich Foods | Green tea, dark chocolate, berries, olive oil | Support good bacteria, reduce inflammation |
By intentionally choosing foods that nurture your microbiome , you’re investing in future health. Probiotic foods add new “good guys” to the microbial mix, while prebiotics nourish and sustain your resident bacteria. Fiber ensures your digestive system stays active, delivering nutrients the microbiota need to thrive. Combined with variety in your meals, these dietary choices create the perfect conditions for a vibrant, resilient gut microbiome .
Gut Bacteria: Spotlight on the Human Gut’s Most Powerful Allies

- Important gut bacteria species, their roles in metabolism, immunity, mental health
Some of the most important bacteria species for human health include Bifidobacterium and Lactobacillus , widely studied for their role in digestion, vitamin synthesis, and immune defense. They ferment dietary fibers, creating short-chain fatty acids that nurture your intestinal lining and curb inflammation. Other microbes like Akkermansia muciniphila support healthy metabolism and weight management by maintaining gut barrier integrity. Emerging research connects certain bacterial strains with improved mood and cognitive function through their influence on the nervous system.
In sum, each species of gut bacteria plays a unique and vital role, and the loss of even a single type can create imbalances (gut dysbiosis) reverberating across the entire body. The key to supporting your gut’s most powerful allies is maintaining diversity and giving them the nutrition they need to thrive.
Microbiome-Risk Factors: What Undermines Gut Health Today?
- Antibiotic use, poor diet, chronic stress, aging’s impact on gut microbiome, environmental toxins

Several risk factors threaten the stability of your gut microbiome —sometimes without you even realizing it. Overuse of antibiotics, even when medically necessary, can wipe out populations of good bacteria along with the bad. A typical modern diet, high in refined sugars and lacking fiber, stifles microbial diversity and encourages the growth of harmful species. Chronic psychological stress alters the balance of hormones and neurotransmitters, influencing microbiota composition and function.
Aging also shifts the microbial landscape, underscoring the importance of ongoing support throughout your life. Finally, environmental toxins—whether from pollution, chemical residues on food, or household cleaning products—can erode your microbiome’s resilience. Identifying and minimizing these risk factors is a core strategy for protecting gut health over the long term.
How to Know if Your Gut Microbiome Needs Help
How do I know if my gut microbiome is unhealthy?
- Symptom tracking, gut health tests, using professional diagnostics
The best way to know if your gut microbiome is struggling is to look for patterns in your health. Track symptoms such as persistent bloating, changes in bowel habits, frequent illness, skin flare-ups, or mood disturbances. These may all be warning signs of gut dysbiosis . If you’re unsure, consider using gut health tests—many now analyze your microbial communities via stool samples, offering detailed reports on bacteria abundance and diversity.
Professional diagnostics, available through clinics and integrative health practitioners, can also help pinpoint imbalances or deficiencies. The Cleveland Clinic recommends listening to your body’s signals and seeking expert advice when symptoms persist. The goal isn’t just to treat existing issues, but to develop a proactive plan for lasting gut health .
Probiotics, Prebiotics and the Microbiome: The Building Blocks of Gut Health
- Difference between probiotics and prebiotics, functions of each in shaping the gut microbiome, recommended sources guided by the Cleveland Clinic
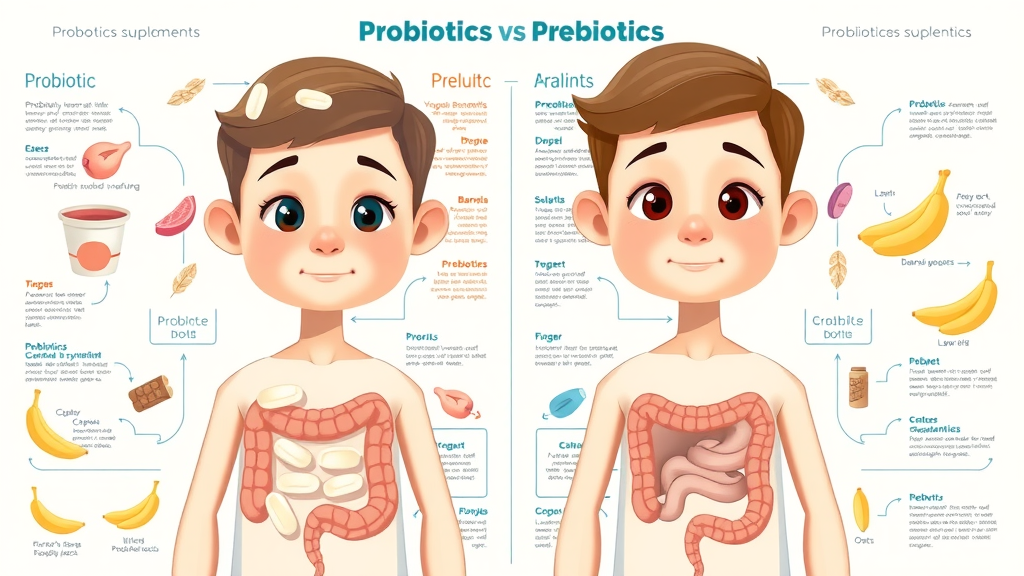
Probiotics are live bacteria that, when consumed in adequate amounts, confer health benefits to the host. Popular sources include cultured dairy (like yogurt and kefir), fermented vegetables (kimchi, sauerkraut), and supplements. They help populate your gut with beneficial species, especially after periods of illness, antibiotic use, or digestive upset. In contrast, prebiotics are non-digestible fibers found in foods such as bananas, oats, garlic, and leeks; they serve as “fertilizer” for your resident microbes, helping them grow and thrive.
Both elements are crucial in fortifying the microbiome, but they function differently: probiotics “seed” the gut, while prebiotics “feed” existing bacteria. The Cleveland Clinic recommends including both in your diet for best results. By combining diverse sources, you optimize your chances of maintaining a flourishing, balanced gut microbiome .
Optimizing Your Microbiome: Top Expert Tips for Long-Term Success
-
Daily Habits to Support Gut Microbiome (Cleveland Clinic’s actionable checklists):
- Eat a rainbow of fiber-rich vegetables every day
- Include a serving of fermented foods with meals
- Minimize processed foods, added sugar, and artificial additives
- Manage stress through mindfulness, exercise, or outdoor activities
- Stay hydrated and prioritize quality sleep
- Avoid unnecessary antibiotics; when needed, use probiotics after treatment
Long-term microbiome health is built on consistency and variety . By forming simple habits and following expert checklists, you hardwire microbial wellness into your daily routine. Regular evaluation of symptoms and gut-friendly nutrition ensures that your “magic” ecosystem stays balanced and vibrant for life.
Check out this engaging animated video for a visual tour of how the gut microbiome communicates with your brain, immune system, and metabolism!
People Also Ask
How can I repair my microbiome?
- Answer: Focus on consuming a diverse and fiber-rich diet, prioritize fermented foods, manage stress, and reduce unnecessary antibiotic use. Probiotics and prebiotics rebuild healthy gut microbiota.
What is the microbiome?
- Answer: The microbiome refers to the community of microorganisms, including bacteria, fungi, and viruses, living in your gut. It’s crucial for digestion, immunity, and overall health.
How do I know if my gut microbiome is unhealthy?
- Answer: Symptoms such as bloating, digestive upset, low energy, frequent illness, and even mood issues can suggest microbiome imbalance.
How do you clean your gut microbiome?
- Answer: Avoid harsh cleanses. Instead, gradually shift toward a plant-based diet, hydrate well, and introduce good gut bacteria through fermented foods and probiotics.
Frequently Asked Questions on Microbiome and Gut Health
-
What are the best ways to test my gut microbiome?
Home test kits based on stool samples or visits to a medical clinic can reveal the diversity and balance of your microflora. Consult a healthcare provider for interpretation and actionable advice.
-
How quickly can the gut microbiome change?
Positive changes often start within a few days of dietary and lifestyle changes, but significant shifts can take 2–4 weeks. Consistency in microbiome-friendly habits makes the biggest difference.
-
Can antibiotics permanently damage my microbiome?
While most healthy microbiomes recover after occasional antibiotic use, repeated courses can cause lasting disruption. Probiotic supplementation and diverse diet help expedite recovery.
-
Which common foods harm gut bacteria?
Processed foods high in sugar, trans fats, and artificial additives feed unhelpful microbes and decrease beneficial bacteria. Limit these for optimal gut health.
Emerging Microbiome Discoveries: What’s Next for Gut Health?
- Latest research on microbiome manipulation, personalized probiotics, and disease-specific gut health therapies
The field of microbiome science is racing forward, with advances in personalized probiotics, gene mapping, and targeted dietary therapies on the horizon. New discoveries are shedding light on how your unique microbial fingerprint could predict responses to drugs, susceptibility to specific conditions, and even your optimal diet for growth and wellness. Stay tuned—the future promises even more sophisticated ways to unlock the magic of your gut microbiome .
Watch this expert-led video as leading scientists separate fact from fiction about the microbiome—ensuring you follow only the best, evidence-based advice for gut health !
Summary: Harness the Power of the Microbiome for Lifelong Wellness
- Restate the crucial role of the microbiome; actionable steps for long-term gut health; inspire readers to take charge of their gut microbiome journey

Your microbiome is the secret to long-lasting vitality and resilience. Embrace fiber-rich foods, embrace diversity, manage stress, and nurture your gut’s “good guys.” By making simple changes today, you lay the foundation for robust health tomorrow. Your gut journey is in your hands—unlock the magic, and you’ll never go back.
Ready for Next-Level Gut Health? Speak to a Microbiome Specialist—Call us +1 817-903-6376
Take the next step—consult with a certified microbiome specialist to create your personalized gut health action plan. Call us at +1 817-903-6376 to unlock your healthiest self today!
 Add Row
Add Row  Add
Add 



Write A Comment