Did you know that over 60% of adults are now turning to collagen supplements in search of smoother skin and better health? The surge in demand for collagen peptides points to a seismic shift in the way people approach skincare, muscle recovery, and overall wellness. If you’ve ever wondered how so many are achieving that radiant glow and joint resilience, the secret might just be hiding in your next smoothie. This comprehensive guide unpacks everything you need to know—helping you make an informed, confident choice about collagen peptides for yourself.
A Startling Statistic: The Growing Demand for Collagen Peptides
The popularity of collagen peptides has soared in recent years, with collagen peptide supplement sales climbing steadily across global markets. As more consumers embrace the benefits of collagen peptides for skin, muscle damage recovery, and holistic wellbeing, the dietary supplement industry is rapidly evolving. Modern research reveals a fascinating trend: collagen peptides aren’t just for beauty enthusiasts—they’ve become mainstream, appealing to athletes, busy professionals, and those simply seeking a more youthful, energized lifestyle.
Recent market analyses and clinical trials highlight how growing scientific credibility and visible effects of collagen have fueled widespread adoption. People are seeking products that offer both cosmetic and health advantages, making collagen supplements and collagen peptide formulations top of mind. As you consider this dietary supplement, understanding where it fits into broader wellness and beauty trends will empower you to choose with clarity.

Collagen Peptides: The Dietary Supplement Revolutionizing Beauty Trends
The beauty and wellness world is experiencing a paradigm shift, led by the extraordinary rise of collagen peptides. Unlike traditional creams and topical solutions, collagen peptides operate from within, harnessing the body's natural processes. As a dietary supplement, they deliver amino acids vital for collagen production and renewal, driving visible changes in skin elasticity and overall health. Individuals embracing this revolution report not just cosmetic improvements, but also faster recovery from muscle damage, enhanced joint function, and stronger hair and nails. No wonder collagen peptide is the most searched nutritional ingredient of the year.
"Over 60% of adults are now seeking collagen supplements for skin health, making collagen peptides the most searched dietary supplement of the year."
What You'll Learn About Collagen Peptides
- How collagen peptides support skin health and muscle repair
- The differences between collagen peptide, collagen supplement, and collagen supplements
- Effects of collagen and what to expect
- How to choose the right collagen peptides for your needs
- Potential side effects and safe usage tips
Understanding What Collagen Peptides Are
Collagen Peptide and Collagen Peptides Defined
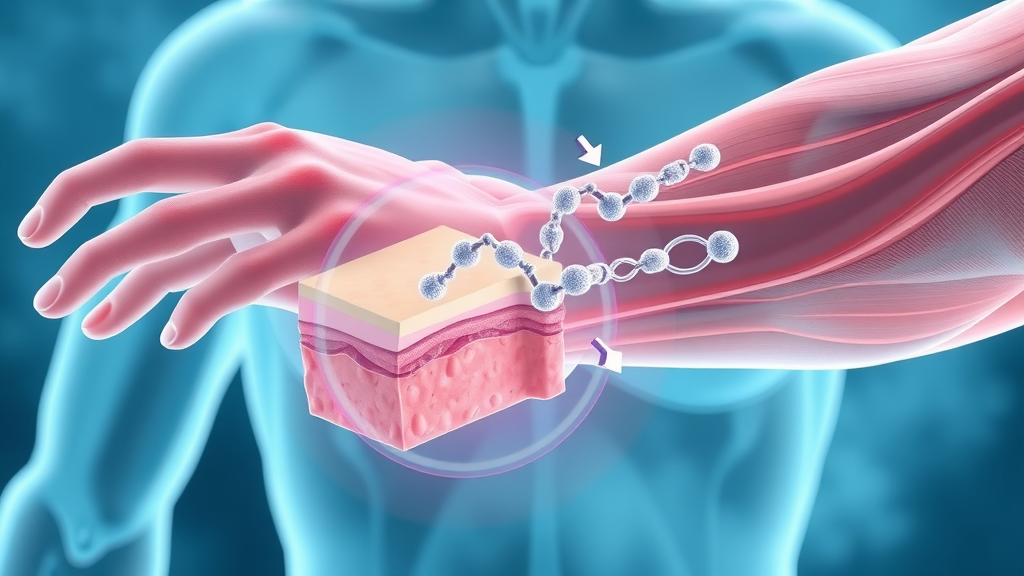
Collagen peptides are short chains of amino acids created when whole collagen proteins are broken down—a process known as hydrolysis. The resulting hydrolyzed collagen peptides are much easier for the body to absorb compared to intact collagen or gelatin. When consumed as a dietary supplement, these smaller peptides circulate throughout the body, becoming the building blocks for connective tissue, skin, and joint repair.
A collagen peptide refers to an individual strand, while collagen peptides generally describes the diverse blend of these chains found in supplements. Most collagen supplements, regardless of the form—be it powder, capsule, or liquid—rely on these hydrolyzed peptides to deliver targeted benefits, like improved skin elasticity and enhanced recovery from muscle damage. Their popularity in the wellness community stems from their bioavailability and proven impact on health through both clinical trial data and everyday testimonials.

How Collagen Peptides Differ from Collagen Supplement and Collagen Supplements
Navigating collagen products can be confusing: what’s the real difference between collagen peptide, collagen peptides, collagen supplement, and collagen supplements? The answer often comes down to specificity and content.
A collagen supplement is a broad term that describes any product containing collagen, whether it is in the form of whole collagen, hydrolyzed collagen (collagen hydrolysate), or targeted peptides. Collagen peptide and collagen peptides are more precise terms indicating products with smaller, highly absorbable protein fragments, typically derived from animal or marine sources.
Most top-rated products focus on low molecular weight peptides, as smaller peptides offer the greatest absorption and biological effect. Manufacturers often tout this feature, citing scientific studies and systematic reviews to distinguish their formulations. As you consider your options, remember: peptides are the gold standard for effectiveness, while “supplement” simply describes the delivery format (capsule, powder, or liquid).
Why Molecular Weight in Collagen Peptides Matters
One of the most important technical factors behind effective collagen peptides is molecular weight. Collagen peptides with a low molecular weight are more easily digested and absorbed in the gut, allowing them to circulate quickly and stimulate collagen synthesis in your skin, muscles, and connective tissue. Recent clinical and controlled trial data show that low molecular peptides deliver more pronounced results compared to larger proteins or gelatin-based supplements.
Scientists use molecular weight as a benchmark for product quality, and the best brands clearly indicate these values on their packaging. If you want fast, visible results—like firmer skin or quicker recovery from muscle damage—opt for supplements featuring hydrolyzed collagen peptides with a low molecular weight.
| Product Term | Main Content | Absorption | Best Use | Typical Form |
|---|---|---|---|---|
| Collagen Peptide | Single small bioactive peptide | Very High | Targeted skin & muscle repair | Powder, capsule |
| Collagen Peptides | Blend of small peptides | Very High | Full-body renewal | Powder, capsule, liquid |
| Collagen Supplement | Hydrolyzed or intact collagen | Medium-High | General maintenance | Powder, capsule, gummies |
| Collagen Supplements | Various forms (may include peptides, gelatin) | Medium | Variety of wellness goals | Powder, capsule, liquid, gummies |
How Collagen Peptides Work in the Body
The Science Behind Collagen Peptides and Their Effects
Collagen peptides are celebrated for their ability to promote collagen synthesis, supporting everything from skin elasticity to resilient joint and muscle tissue. After you ingest a collagen supplement, digestive enzymes break the peptides into amino acids and specific bioactive sequences. These circulate in the bloodstream and are quickly incorporated into skin, cartilage, and muscle fiber repair.
Multiple systematic reviews and randomized controlled trial studies support that oral collagen supplementation increases the density of collagen in the skin, helping maintain a youthful appearance and smoother texture. For physically active individuals, regular collagen peptide supplementation can accelerate recovery from resistance exercise and reduce the intensity of muscle damage after workouts. The impact goes beyond beauty—collagen peptides also benefit connective tissue, joint health, and overall physical performance.
Effects of Collagen: From Younger Skin to Reduced Muscle Damage
Research consistently links collagen peptides to a range of impressive benefits. Increased skin elasticity is often the first visible sign, followed by improvements in connective tissue and reduced post-exercise soreness. A high-quality collagen supplement doesn’t just target wrinkles; it works systemically, providing amino acids essential for muscle repair, bone density, and even the health of your gut lining.
Athletes and active individuals find collagen peptide supplementation particularly effective for minimizing muscle damage from high-intensity workouts or resistance training. It’s no wonder that wellness experts and dermatologists alike recommend this powerhouse ingredient for anyone seeking comprehensive benefits—not only for beauty but for whole-body resilience.
- Increases skin elasticity
- Supports connective tissue
- Aids in muscle recovery
- Promotes joint health
Top Features and Benefits of Collagen Peptides
Collagen Peptides for Skin: Achieve Youthful, Firm Skin
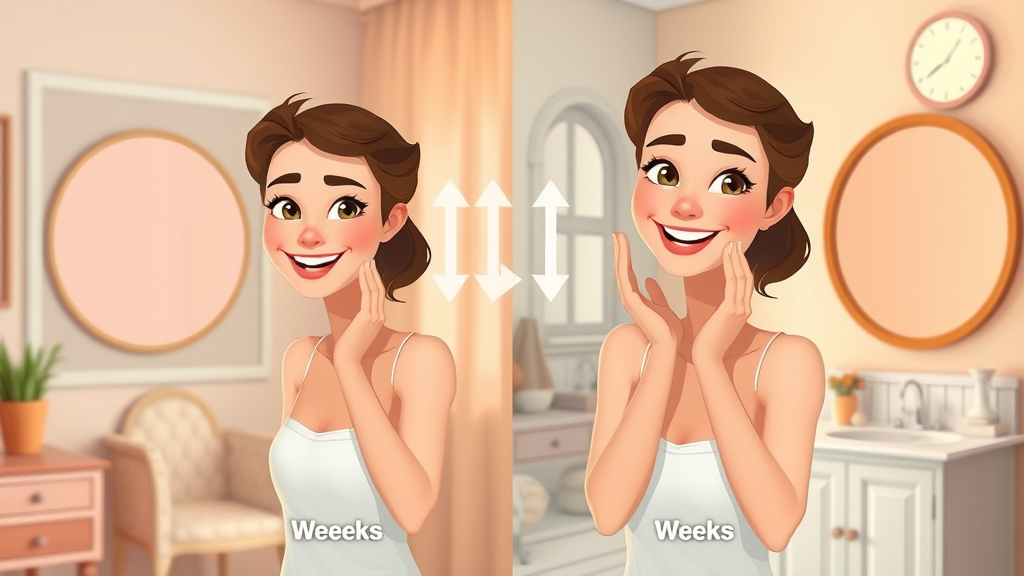
The cornerstone benefit of collagen peptides is their remarkable impact on skin quality. By providing the necessary amino acids for collagen biosynthesis, they enhance skin elasticity and firmness, while also smoothing out fine lines and wrinkles. Numerous clinical trials and systematic reviews have confirmed that daily collagen supplementation can deliver visible improvements within weeks, especially in adults facing collagen loss due to aging or environmental stressors.
Unlike topical products that act only on the surface, a collagen peptide supplement nourishes your skin from within, supporting better hydration and resilience. Users and dermatologists often report a fresher, more luminous complexion—the true mark of healthy, youthful skin.

Muscle Damage Recovery and Collagen Peptides
Collagen peptides don’t just maintain beauty—they are a powerful aid in muscle recovery, particularly after exercise. When you engage in resistance or endurance exercise, tiny tears occur in muscle fibers (muscle damage) that require effective repair mechanisms. Supplementing with collagen peptides supports this process by supplying the amino acids necessary for rebuilding tissue, reducing inflammation, and minimizing soreness.
Clinical and controlled trials have demonstrated that those who incorporate collagen peptide or hydrolyzed collagen supplements post-workout experience enhanced recovery and are less likely to develop joint stiffness and pain. This makes collagen peptides an excellent addition not only for athletes but for anyone managing an active lifestyle or recovering from injury.

Boosting Nail, Hair, and Joint Health with Collagen Supplements
The power of collagen supplements goes well beyond skin and muscle. By enhancing collagen production, these supplements promote healthier, stronger nails and thicker, more resilient hair. People who experience brittle nails or thinning hair often notice pronounced improvements within months of starting consistent collagen peptide supplementation.
Moreover, the positive impact on joint health is invaluable. As a crucial component of cartilage and connective tissue, collagen peptides help reduce joint discomfort, improve mobility, and even support overall bone density. It’s this wide range of benefits that has made collagen supplements a core component of holistic beauty and wellness routines.
"Collagen supplements have become a cornerstone in holistic beauty routines for their proven effects on skin health." – Industry Expert
Types of Collagen Peptide Products
Powder, Capsules, and Liquid Collagen Supplements
Today’s market offers a variety of collagen peptide products to fit every preference and lifestyle. The powder form—arguably the most popular—mixes easily into coffee, smoothies, or water and allows for precise dosage customization. Capsules offer convenience for those on the go or those who prefer not to taste their supplements. For rapid absorption, liquid collagen has gained traction, delivering bioactive peptides directly to your system with minimal digestion.
Each format contains the same essential low molecular weight peptides, but considerations around dosage control, flavor, portability, and absorption speed can guide your choice. Some brands even blend collagen with vitamin C, hyaluronic acid, or other synergistic ingredients to enhance results.

How to Choose the Best Collagen Supplement for Your Needs
Selecting a collagen supplement should be guided by your primary wellness goals and lifestyle needs. First, prioritize products that list low molecular weight collagen peptides and include transparent sourcing and third-party testing. Check for additional bioactives (like vitamin C) that support collagen synthesis, and avoid unnecessary fillers or artificial ingredients.
If your focus is skin health, opt for a powder or liquid that can be easily incorporated into your daily routine. For muscle damage recovery or connective tissue support, look for supplements specifically mentioning peptide supplementation for athletes. Always follow the indicated daily dosage, and consult a healthcare professional if you have allergies or special medical needs.
Experience the transformation visually! Watch this short video showcasing how collagen peptide supplementation enhances skin elasticity, revealing real before-and-after results. See animated overlays that clarify how peptides are absorbed and put to work for your skin.
Watch: Collagen Peptides in Action for Skin Health
Seeing is believing. This video dives into the process of collagen peptide absorption and the visible improvements users report—from smoother lines to firmer, more youthful skin. Enjoy expert commentary and vibrant animations that simplify complex science, making the benefits of collagen clear and compelling for all viewers.
Compare top-rated collagen peptides with insights from nutritionists and healthcare professionals. This feature highlights product purity, efficacy, and consumer feedback—helping you select the brand that aligns with your goals and budget.
Pricing and Where to Buy Collagen Peptides
Comparing Collagen Peptide Brands: Value, Quality, and Reviews
Deciding on a collagen peptide brand involves more than checking price tags—look for transparent ingredient sourcing, reputable certifications, and real customer reviews. Some products fetch a premium due to added nutrients or patented hydrolysis techniques that promise smaller, more effective peptides.
Value often correlates with reviews and clinical backing, so consider brands with substantiated claims and testimonials. Whether buying online or in-store, always look for a clear breakdown of peptide content, recommended dosage, and lab testing details to ensure maximum results and safety.

| Brand | Form | Key Features | Price (30-Day Supply) | Consumer Rating |
|---|---|---|---|---|
| GlowVital | Powder | Low molecular, blended with vitamin C | $38.99 | 4.8/5 ⭐ |
| FlexActive | Capsule | Highly purified, no fillers | $32.50 | 4.6/5 ⭐ |
| PureMarine | Liquid | Marine source, ultra-absorbable | $45.00 | 4.7/5 ⭐ |
| EssentialPeptide | Powder | Grass-fed, unflavored, highly soluble | $29.99 | 4.5/5 ⭐ |
How to Use Collagen Peptides for Best Results

To see optimal results from your collagen peptides, consistent and correct usage is key. Begin by selecting a product that matches your wellness goals—verify the dosage and source for best compatibility. Always mix powders thoroughly, preferably with a meal or beverage, to improve absorption.
Combine your supplement with a balanced diet rich in vitamins and minerals, as nutrients like vitamin C play a crucial role in collagen synthesis. Monitor your body’s response for several weeks, making note of visible changes or improvements in joint and muscle comfort. Adjust your intake as needed and consult a healthcare professional if you experience digestive upset or are using other medications.
- Select the right collagen peptide product for your goals
- Follow daily dosage recommendations
- Combine with a balanced diet for maximum efficacy
- Monitor effects and adjust intake as needed
What to Expect: Effects of Collagen and Visible Signs of Change
Timeline for Collagen Peptides Results: First Signs and Long-Term Gains
When starting with collagen peptides, patience pays off. Most users notice initial subtle changes—such as improved hydration and plumper skin texture—within three to four weeks of regular use. More dramatic improvements in skin elasticity, hair and nail strength, and post-exercise recovery can take two to three months, especially if combined with other healthy lifestyle choices.
Long-term gains, such as smoother wrinkles, better mobility, or resilience against muscle damage, result from ongoing supplementation and sustained collagen synthesis. Remember, individual results vary based on factors like age, baseline health, and adherence to recommended dosages.
Are There Side Effects to Collagen Peptides?
Side Effects and Safety Tips for Collagen Peptide Users
While collagen peptides are generally considered safe for most people, some may experience mild digestive discomfort or, in rare cases, allergic reactions—especially if the product contains fish, shellfish, or other allergens. Following the recommended daily dosage greatly minimizes risk, and it’s always wise to consult a healthcare professional before starting any new dietary supplement.
Monitor your response during the first month. If you notice persistent upset, discontinue use and seek guidance. Safe supplementation is about quality as well as quantity—choose reputable brands with transparent labeling and robust customer support.
- Digestive discomfort
- Allergic reactions
- Safe daily dosages
Frequently Asked Questions about Collagen Peptides

What do collagen peptides do for a person?
Collagen peptides help increase your body's collagen levels, supporting skin elasticity, joint health, and muscle repair. As highly absorbable amino acid chains, they provide the foundational proteins your body uses to maintain and rebuild connective tissue, hair, nails, and bones. This results in younger-looking skin, reduced joint pain, faster muscle recovery, and an overall boost to physical resilience and appearance.
What happens if I take collagen peptides every day?
Taking collagen peptides daily helps keep your body’s collagen supply at optimal levels. With consistent use, you’ll likely notice improved skin texture, stronger hair and nails, and lower incidence of muscle damage from exercise. For many, regular supplementation also leads to fewer joint aches and better mobility. As with any dietary supplement, results may vary, so monitor your progress and adjust intake as needed.
What are the first signs that collagen is working?
The initial benefits of collagen peptides often appear as increased skin hydration and smoothness within the first few weeks. Many also report stronger fingernails and a decrease in joint and muscle soreness. Over time—typically within 8–12 weeks—noticeable improvements in skin firmness, reduced fine lines, and enhanced post-workout recovery begin to emerge, indicating that your body is effectively utilizing the peptides.
Are there side effects to collagen peptides?
Side effects from collagen peptides are rare but can include mild digestive upset or, in sensitive individuals, allergic reactions. To minimize risk, start with the recommended serving and choose products with transparent ingredient lists. Most healthy adults tolerate collagen supplements well, but if you have allergies or underlying health conditions, always seek guidance from a care professional before beginning supplementation.
- Collagen peptides help maintain skin and joint health, with a range of appearance and wellbeing benefits.
- Daily supplementation encourages ongoing collagen production for visible results.
- First improvements usually show within weeks as skin feels more hydrated and vibrant.
- Side effects are rare and typically mild, especially with high-quality products.
Key Takeaways: The Power of Collagen Peptides
- Collagen peptides offer wide-ranging benefits for skin, muscle, and joint health
- Choosing the right form and brand is crucial for best results
- Visible effects of collagen peptides can often be seen within weeks
- Side effects are rare but should be monitored, especially for allergies
Conclusion: Make the Youthful Choice with Collagen Peptides
Why Collagen Peptides Are a Smart Investment in Skin and Wellness
Investing in collagen peptides is an actionable, science-supported way to boost your skin, joint, and overall wellness. With evidence mounting from both clinical studies and everyday users, there’s never been a better time to experience the magic of collagen peptide supplementation firsthand.
Ready for Youthful Skin?

Call Katrice 555.555.5555 for Your Collagen Peptides Consultation
Want personalized advice or ready to choose your collagen peptides? Visit www.Katrice.com today and take the next step toward glowing, youthful skin.
 Add Row
Add Row  Add
Add 



Write A Comment